Written by: Elizabeth Merritt
Celebrating the launch of telehealth services that will increase access to quality health care.
Bamberg, S.C., March 29, 2023 – Palmetto Care Connections (PCC), a non-profit organization that brings technology, broadband, and telehealth solutions to health care providers in rural and underserved areas in South Carolina, celebrated the launch of telehealth services at the Bamberg County Office on Aging in Bamberg, S.C. on Monday, March 27.
“We are so proud of the work that we do and are always looking to do more,” says Bamberg County Office on Aging Director Kay Clary. “To start telehealth is exciting for us. I hope that the seniors will take advantage of it and I feel like it’s moving us more towards the future in this area. We are pleased to be working with Palmetto Care Connections with the installment of telehealth and hope our community enjoys it.”
Event speakers included Director Kay Clary of Bamberg County Office on Aging, Connie Munn, Director of South Carolina Department on Aging, South Carolina Lieutenant Governor Pamela Evette, South Carolina State House Representative Mark Smith, South Carolina Senator Brad Hutto, and Kathy Schwarting, Chief Executive Officer of PCC.
“As we know, particularly with Bamberg, many areas in South Carolina are rural and we’ve seen the hospitals close. To be able to have that type of telehealth offered here at the Bamberg Office on Aging is phenomenal,” says Connie Munn, director of the South Carolina Department on Aging.
Representative Mark Smith, along with Senator Brad Hutto, presented a house resolution honoring and celebrating Palmetto Care Connections for increasing medical care to the underserved.
“It has taken public-private partnership to make this happen today. This is a beautiful example of how it can work beautifully when executed well,” says Representative Mark Smith.
Providing quality health care could not be possible without internet access. Keynote Speaker and South Carolina Lieutenant Governor Pamela Evette recognized the importance of getting broadband out to rural areas to address the needs of South Carolina citizens.
“I am proud to tell you that over the course of the post-pandemic we’ve spent $480 million getting broadband out to our rural areas. Money that will take broadband down to the last mile,” says South Carolina Lieutenant Governor Pamela Evette.
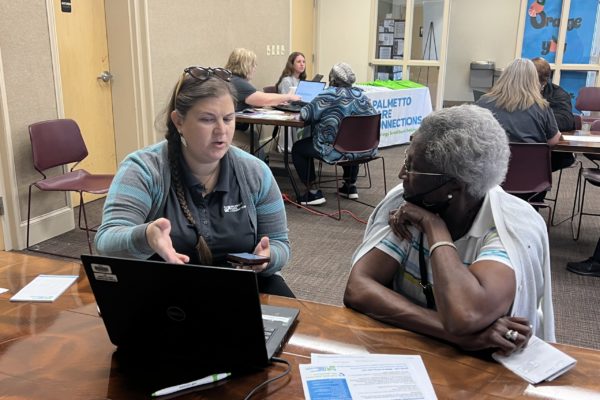
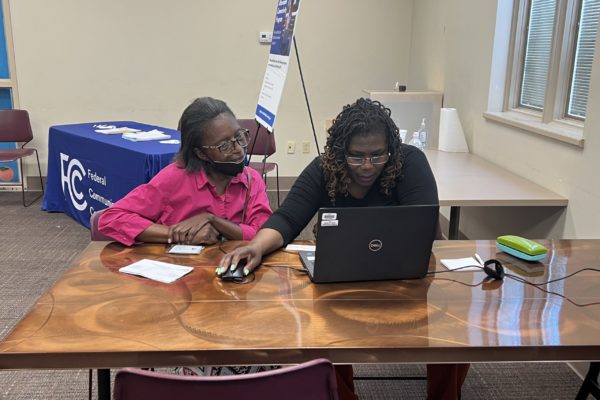
The launch of telehealth services at the Bamberg County Office on Aging also celebrates the seniors who have learned how to use telehealth through PCC’s Digital Literacy program.
“We have today trained over 1,000 rural and underserved residents in South Carolina,” says Kathy Schwarting, chief executive officer of PCC. In 13 counties, we’ve given out over 1,000 devices and we’ve helped over 1,000 people get Internet access; that is very important to us.”
For more information on Palmetto Care Connections, visit https://www.palmettocareconnections.org/.
###
About Palmetto Care Connections
Established in 2010, Palmetto Care Connections (PCC) is a non-profit organization that brings technology, broadband, and telehealth solutions to health care providers in rural and underserved areas in South Carolina. PCC assists providers in keeping health care local and increasing quality services to underserved South Carolinians. For more information, visit https://www.palmettocareconnections.org/.
Website: https://www.palmettocareconnections.org/
Facebook: https://www.facebook.com/palmettocareconnections/
Instagram: https://www.instagram.com/palmettocareconnections/
Twitter: https://twitter.com/palmettocaresc
LinkedIn: https://www.linkedin.com/company/palmetto-care-connections/