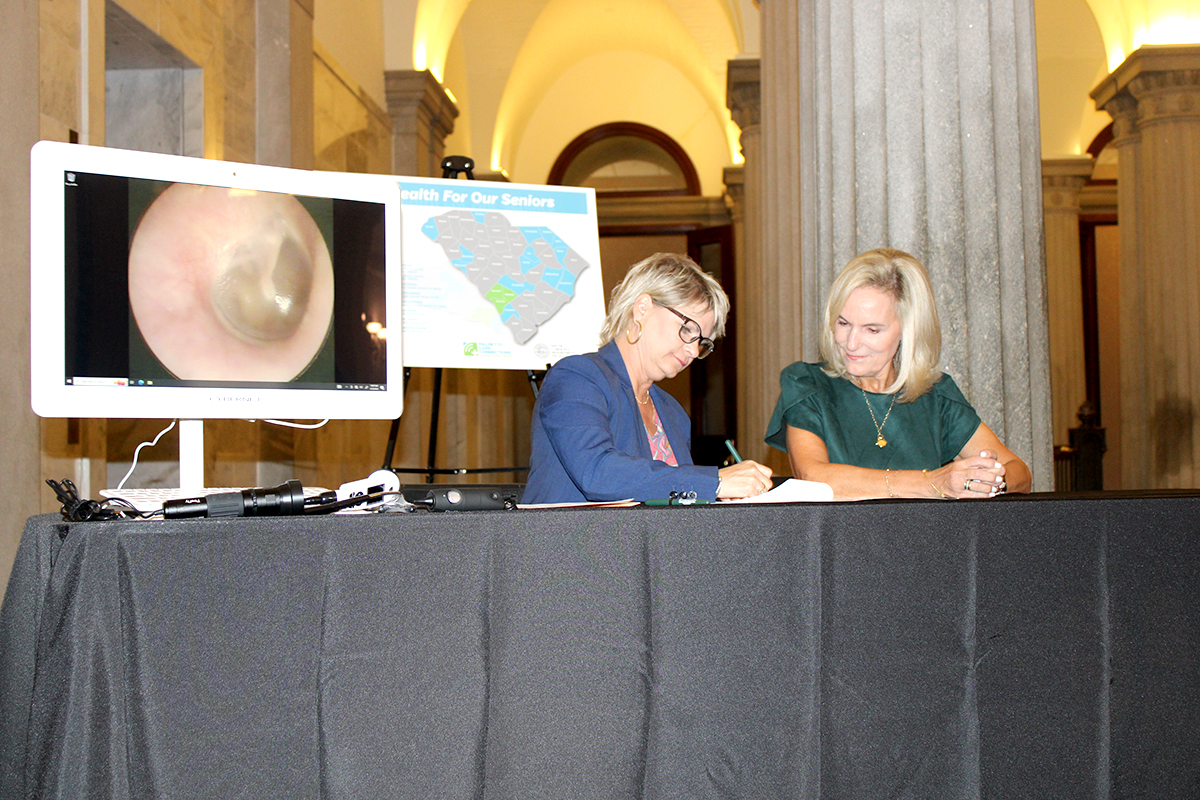
Pictured (L to R): Kathy Schwarting, CEO, PCC and Connie Munn, Director, SCDOA
Photo Credit: SC Department on Aging
PCC, Department on Aging Announce Statewide Expansion of Telehealth
Up To 18 Health Offices To Be Assessed For Innovative Telehealth Carts
COLUMBIA, S.C. – Palmetto Care Connections (PCC), a non-profit telehealth network serving
rural and underserved communities across South Carolina, and the South Carolina Department
on Aging (SCDOA) today celebrated the ceremonial signing of a Memorandum of Agreement
expanding access to telehealth care for thousands of South Carolinians.
Led by Chief Executive Officer Kathy Schwarting, MHA, a full staff and a board of directors
including health care leaders from across the state, PCC will conduct site assessments at up to
18 rural senior centers to determine each office’s telehealth readiness and broadband
capabilities. Each office will then receive a telehealth cart for area seniors to use for telehealth
visits. The carts, provided by PCC for deployment, would be available for those who may
otherwise not have adequate access to health care.
“The people of our state deserve access to the highest quality health care,” said Schwarting.
“Collaborating with Director Connie Munn and her impressive team at SCDOA we have done
great work and made significant progress toward putting telehealth carts in offices across South
Carolina. Once we have these telehealth carts in place, the underserved and vulnerable among
us will be able to benefit from broad scope of health services, which they need and deserve. We
thank members of the General Assembly and the entire team at Aging for working so well with
us to make this next step a reality.”
“With our growing older population in South Carolina, at the Department on Aging, our focus is
to ensure that our older adults have a place to live, have quality of life, and can age with dignity
and respect,” Munn said. “We are grateful for the partnership with Palmetto Care Connections
that will improve access to healthcare which is vital to the quality of life for our older adults.
These telehealth carts will be able to provide a critical role in the wellness of older adults. This
would not be possible without the support from Kathy Schwarting and her dedicated team, and
the members of the General Assembly to help provide our aging population this invaluable
resource to healthcare.”
Once offices are identified as suitable for telehealth carts and PCC and SCDOA have placed
carts at the locations, PCC will train staff members to assist their seniors in successfully
completing a telehealth visit, and share online educational offerings to staff members at each
location. Additionally, PCC will provide ongoing support for each telehealth cart and help
promote the new telehealth service.
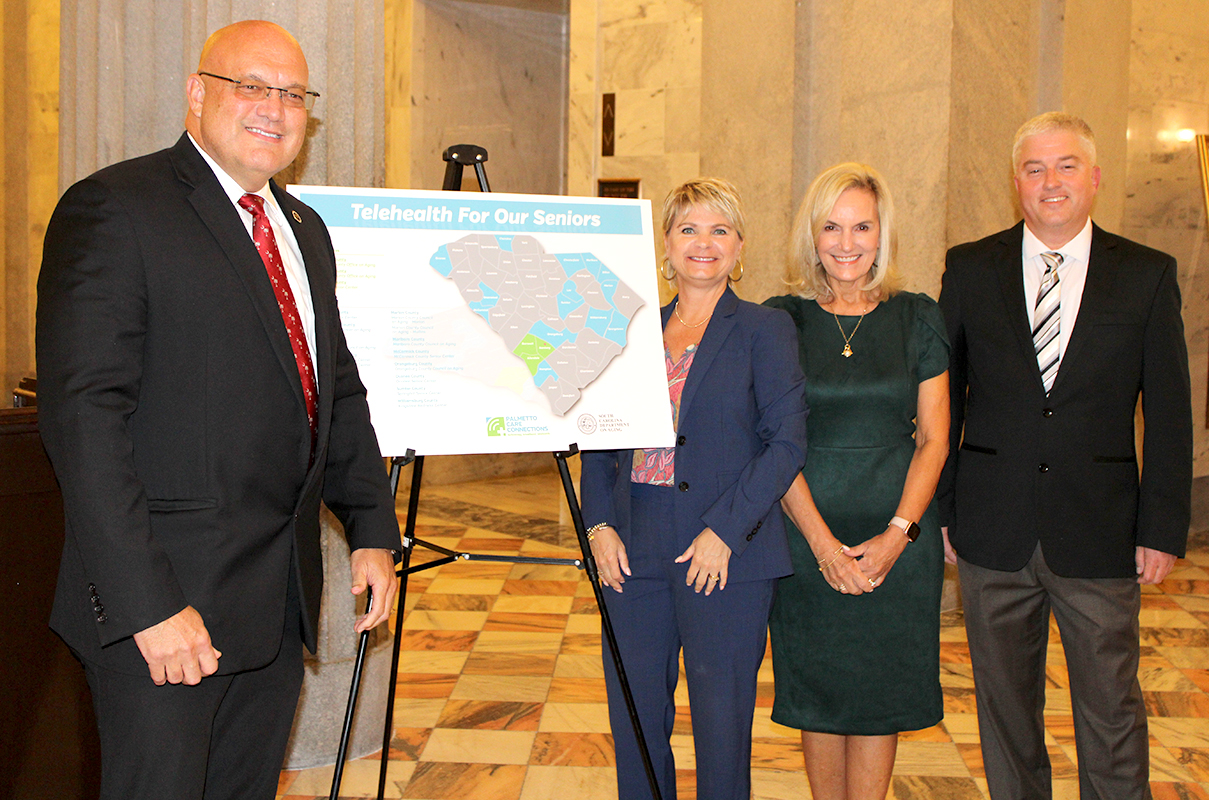
Pictured (L to R): SC Representative Mark Smith, Kathy Schwarting, CEO, PCC, Connie Munn, Director, SCDOA, and Matt Hiatt, Chief Technology Officer, PCC
SCDOA’s mission is to meet the present and future needs of seniors, and to enhance their
quality of life in South Carolina. Through a network of regional Area Agencies on Aging and
local organizations SCDOA develops and manages services that help seniors remain
independent in their homes and communities.
Established in 2010, Palmetto Care Connections (PCC) is a non-profit organization that brings
technology, broadband, and telehealth solutions to health care providers in rural and
underserved areas in South Carolina. PCC hosts the Annual Telehealth Summit of South
Carolina presenting state and national best practices and trends, as well as providing
networking connections for health care, technology and broadband professionals.
The leader of the South Carolina broadband consortium, PCC assists health care providers in
receiving broadband savings through the Federal Communication Commission’s Healthcare
Connect Fund program. Since 2013, PCC has helped providers save more than $30 million in
broadband costs.
-###-







![IMG_0379[478426] IMG_0379[478426]](https://www.palmettocareconnections.org/wp-content/uploads/2023/07/IMG_0379478426.jpg)




