DHEC makes vaccine available to anyone that wants it
Click Here to Listen to the story
Getting a COVID-19 vaccine appointment requires going online. But plenty of South Carolinians are not connected.
At the end of March, 2021, COVID-19 has killed more than 9,000 people in South Carolina, and almost 8,000 of them are people above the age of 60.
Reconcile that with the Pew Research Center’s findings that once above the age of 60, access to and ownership of smartphones or any device connected to the internet drops sharply as age increases.
Where this overlaps dangerously is in the middle of the COVID vaccine rollout, which requires residents to register through their phones, tablets, or computers. In a state where broadband access is being addressed more urgently by federal and state officials, huge parcels of South Carolina between Newberry and Jasper counties still have zero access to the internet, according to coverage maps by Palmetto Care Connections (PCC), a nonprofit advocate for equitable and wide-reaching broadband access in the state.
Kathy Schwarting, CEO of PCC, says that this puts residents – particularly rural seniors – in a bad spot.
“There’s the access issue,” Schwarting says. “Whether or not your area even has the ability to have internet. If you live out in the country, outside of the city limits, you may not even have fiber; and it’s very expensive to run it.”
But there’s also an age issue, remember. The Pew study shows that in 2017, the last year data is available, 67 percent of seniors were on the internet but 51 percent had access to broadband. Those numbers are likely a combination of choice and circumstance and may have changed in the intervening years, but there are, nevertheless, seniors who are simply not connected, at a time when the way to get registered for a COVID vaccination is online.
Schwarting has an aunt in her 70s who wanted to get vaccinated and had to call the South Carolina Department of Health and Environmental Control (DHEC) on the phone. The department initially told her she needed to sign up online, but Schwarting’s aunt has no computer and no internet-capable phone.
Schwarting says DHEC brought her aunt into an office and registered her in person. And while she’s happy it worked out for her aunt, Schwarting knows not everyone who’s offline will be able to do that. For rural seniors in particular, physically getting to a DHEC office could be a near impossibility.
Schwarting says several seniors without email addresses or even a connection have enlisted help from their children and grandchildren to register. For those who can get that kind of help, great, but again, she says, not everyone has someone connected whom they can call upon for help.
Cost, of course, is another issue. Even with access to some kind of reliable internet, it can be expensive. High-speed internet, which is often needed to navigate websites these days, is considered anything above 25 megabytes per second. Some plans in South Carolina run at 300mbs. The more mbs, the more money.
Monthly plans for low-income residents can start at $10 (or in some cases be essentially free). Some providers temporarily expanded eligibility to broadband because of the pandemic.
AT&T, one of the major providers in the state, did this. Lead Public Relations Manager Megan Daly said in a statement to South Carolina Public Radio that the company’s Access from AT&T program was offered to households participating in the National School Lunch Program and Head Start, “for $10 a month or less. Also, for a limited time, customers at locations with available AT&T Internet speeds above 10 Mbps may be eligible for a speed upgrade up to 25 Mbps.”
But if you don’t qualify for a low-income plan, broadband service can be pricy. It’s not unusual for South Carolinians to have plans costing around $75 a month in some well-connected areas. And, of course, plans expanded because of the pandemic will not be permanent, which, Schwarting says, could become problematic for unconnected lower-income residents looking to access medical records or find work after life moves past COVID’s disruption.
“If you are living paycheck-to-paycheck,” she says, “and you are trying to balance getting your medications, paying your light bill, paying your mortgage, making sure you have groceries, $75 is an awful lot of money. And [a $15] increase is a lot of money in a house where they don’t have extra money.”
According to BroadbandNow, South Carolina ranks 31st among U.S. states in high-speed connectivity, and about 53 percent of residents have access to a wired, low-price plan.
Connecting with the Unconnected: ‘Word of Mouth is Powerful’
An unexpected side-effect of the pandemic is that for as much as it put a spotlight on the need for technology access, it also reminded us that we still need analog options for getting in touch with people in a crisis.
Social media is the favored distribution method of health agencies, social services workers, news companies, and whoever else wants to get the word out about something. The reach is immense and immediate, but it does zero good for anyone who isn’t connected.
“Boots on the ground,” says Davia Smith, PCC’s director of education. “Social media works for some but it doesn’t work for all.”
Smith says that meeting people where they live – the grocery stores, churches, pharmacies – is the key to getting through to communities that might be cut off. That includes poor communities, communities of color, and rural neighborhoods, which all share something important to remember – a tendency to trust most in people they already know personally.
Getting to people in these communities is a clearly hefty task. But Smith says it’s necessary, especially in light of the continuing disappearance of one particular source of information.
“You have some communities that no longer have a local newspaper,” she says.
And even in places where local papers still exist, they are usually weeklies, which Smith says can create troublesome lags when people need to receive urgent information. So social and health workers, she says, need to ramp up their alternatives for how to get information to residents, and need to stop thinking that a website or an app solves every problem.
“We can’t stay behind the computer screen and expect everything to get done,” she says. “Word of mouth is powerful.”
DHEC, for its part, appears to have learned this lesson some.
In a statement, DHEC said:
We work to get current messaging to people who don’t rely on the internet for their news and information by way of:
- signage at gas stations (targeted rural areas)
- billboards (target rural areas)
- advertisements in every weekly newspaper in the state
- radio PSAs
- TV PSAs
- direct mailers
- ongoing partnerships with local organizations that promote our messaging within their communities
- continued partnerships with our state’s faith-based organizations to help share important information and resources
- We partner with the nonprofit Hold Out The Lifeline (HOTL) to support grassroots statewide efforts directed toward African American churches and community groups. Among the many services offered, HOTL is conducting virtual briefings, distributing some of DHEC’s hardcopy resources and materials, and distributing PPE (face masks, hand sanitizer, gloves etc.) HOTL also provides church leaders with a toolkit to help them plan educational sessions that help inform their members about COVID-19 and COVID-19 vaccine. In January alone, it’s estimated that HOTL reached nearly 30,000 congregants with current DHEC messaging.
- information at public transit hubs
- shared information with the S.C. Department of Commerce and DHEC’s regulated business community to share with employees (breakroom signage and take-home literature)
- sharing information and resources with the S.C. Commission for Minority Affairs, S.C. Department of Aging, Office of Rural Health, S.C. Department of Employment and Workforce, AARP, PASOS, housing authorities, public transportation systems, etc., to share current key messaging and phone numbers for accessing additional information.
Smith sympathizes with anyone trying to get real information out to communities that aren’t as well-connected. She says that between misinformation, constant updates of real information about what’s safe or where and when a vaccination event will happen, and the sheer volume of information hitting people (especially, ironically, the connected), getting good information through to residents is a tall task, but one that demands getting done right.
She says that as tech access becomes more ubiquitous, it will be important to remember that tech is not a Messiah, but a tool.
“I remember when stores … put in the U-Scan™ registers, and it was like, ‘Technology is going to take everyone’s job,” she says.
That didn’t happen, of course, and that’s her point.
“COVID has shown us that technology is a useful tool, but it’s not going to replace everything,” she says.
Efforts to Expand Access
One positive thing about the pandemic is that its main lesson about internet access – that it’s not a luxury anymore, but a necessity – appears to have gotten through to lawmakers who could do something about it.
Both of South Carolina’s U.S. Senators, Lindsey Graham and Tim Scott, Republicans, co-sponsored the Governors’ Broadband Development Fund, along with Sen. Mark Warner, Democrat, of Virginia. In December, the Federal Communications Commission granted the measure $121 million to expand rural broadband in South Carolina. The bill aims to get access to almost 109,000 homes that otherwise, according a statement Graham made, “might as well be on the moon when it comes to getting high-speed internet service.”
In mid-January, the outgoing Trump administration announced a $1.6 million grant to the Lancaster Telephone Company to deploy a fiber-to-the-premises network to connect 5,574 people, 20 businesses, 17 farms, and three educational facilities to broadband in Lancaster and Chester counties.
While measures like these certainly can help, South Carolina still has quite a way to go. The State newspaper reported last June that connecting all of South Carolina could be an $800 million endeavor. An ambitious plan introduced by U.S. Rep. and House Majority Whip Jim Clyburn (D, SC-6th), the Accessible, Affordable Internet for All Act, looks to invest $100 billion to build high-speed broadband infrastructure in unserved and underserved communities all over the country.
That bill was introduced last June and is making the rounds among the Biden administration’s American Rescue Plan.
And South Carolina’s state leaders have looked to tackle the issue of broadband access as well. In September, Gov. Henry McMaster signed the GREAT (Growing Rural Economies with Access to Technology) program into law. It looks to set the stage for a codified broadband access law in the state.
And the state’s 2021 budget features a $30 million safeguard to expand rural broadband to schools and businesses.
All of this is good news to guys like Graham Adams, CEO of the South Carolina Office of Rural Health (SCORH), who says that one of the pandemic’s few positives is the attention broadband access to rural America has gotten.
“[It’s] a much more recognized problem,” Adams says. “There’s a lot more attention on the lack of broadband in rural communities. The whole world was thrown into telecommuting and tele-learning; we all gained a greater appreciation for the importance of connectivity in the home.”
Something Adams hopes people in general come to understand better as access accelerates is that rural communities do want broadband. He says it’s not a matter of not wanting so much as a matter of simply not having access nor the ability to pay for it.
For now, he is glad to see progress being made, including in efforts like the joint SCORH, PCC, South Carolina Rural Innovation Network effort to map access points in Barnwell and Williamsburg counties. Those are two areas plagued by lesser tech access and lesser tech literacy, which Adams also says needs to be a major component of broadband expansion – because tech access won’t do anyone any good if no one can afford it and if no one knows how to use it.
A Small Data Snapshot
The caveat with this section and its accompanying graph is, don’t try to apply it too broadly. But as a way of illustrating a piece of the intersection of age, access, and vaccination, the data points do show a couple interesting things, as of March 26, 2021.
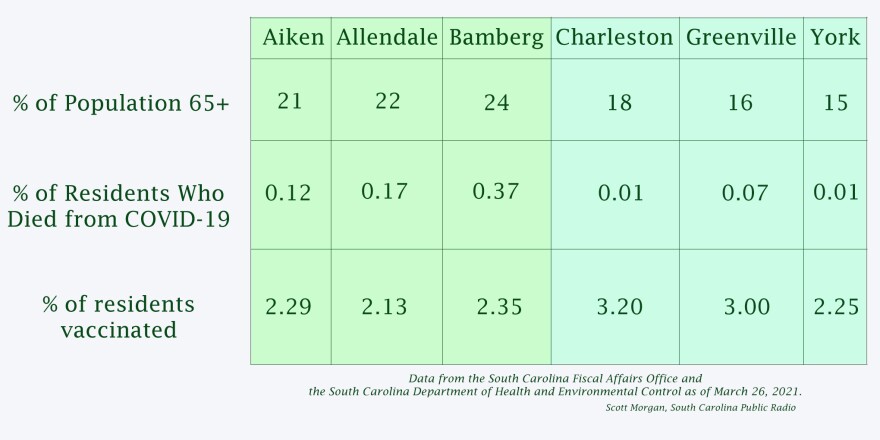
Allendale, Aiken, and Bamberg counties, all mostly rural, have some of South Carolina’s largest areas without internet coverage; they each also have, according to data from the South Carolina Fiscal Affairs Office, senior populations above 20 percent – and, according to data from DHEC, have higher rates of death from COVID compared to three of the most connected counties in the state, Charleston, Greenville, and York. All three of these counties have senior populations below 20 percent.
While the dataset is too small to extrapolate any sweeping trends, there are also some correlations between how wired a county is and the percentage of that county’s residents who have been vaccinated at least once. Only York County, which is highly connected but has a relatively low vaccination rate, stands apart.
Addendum, March 26, 2021: On the day this story published, U.S. Senators Lindsey Graham and Tim Scott of South Carolina announced the $20 billion State Fix Act to build 5G fiber infrastructure in underserved rural communities.
If signed into law, the APTA-backed bill would achieve a major association goal. Contact Congress now to voice your support.
Informed by lessons learned during the COVID-19 pandemic, a bipartisan group of lawmakers in the U.S. House of Representatives has introduced APTA-backed legislation that would make payment for services delivered via telehealth a permanent option for PTs and PTAs participating in Medicare. If passed into law, the legislation would represent a major shift in payment policy long advocated by APTA.
Known as the Expanded Telehealth Access Act (H.R. 2168), the bill was initially sponsored by Reps. Mikie Sherrill, D-N.J., and David McKinley, R-W.Va. The proposed legislation rapidly gained additional support from both parties, and by the time of its introduction it included 14 additional original cosponsors. The association is urging all PTs, PTAs, students, patients, and other supporters to contact members of Congress by way of the APTA Patient Action Center to voice their support for the new bill.
Essentially, the bill would instruct the U.S Centers for Medicare & Medicaid Services to permanently adopt what is a temporary waiver of restrictions on payment for telehealth delivered by PTs and PTAs, occupational therapists, occupational therapy assistants, speech-language pathologists, and audiologists. The Secretary of Health and Human Services also would be allowed to further expand the list of authorized telehealth providers.
The inclusion of PTs and PTAs as authorized to provide services via telehealth to Medicare beneficiaries has been a longtime advocacy focus for APTA, dating back years before the pandemic triggered the CMS decision to invoke so-called 1135 waivers to allow for payment.
In a press release announcing the introduction of the bill, the primary cosponsors point to the effectiveness of telehealth during the pandemic as an indication that the approach can work for PTs, OTs, and other providers.”During the COVID pandemic, healthcare providers adapted and provided telehealth services to serve the needs of millions of vulnerable Americans,” said Rep. McKinley in the release. “Telehealth services have been beneficial to the health and well-being of America’s seniors and after the public health emergency ends, it’s crucial that critical access to telehealth does not abruptly end.”
“The use of telehealth services during this crisis has demonstrated the critical role technology can play in improving health equity,” said Rep. Sherrill. “No one should have to go without care when a video or phone conversation with a health care provider could mean quicker, safer medical attention.”
APTA President Sharon L. Dunn, PT, PhD, applauded the bill on behalf of the association, saying that “the use of telehealth during the pandemic has helped ensure patient access to physical therapist services, minimize potential exposure to the virus, and provided an option for therapy clinics and their patients during quarantine restrictions — and it’s made it all the more clear just how valuable telehealth is to patients who may need alternative access to therapy.”
“Passage of this bill would represent a major win for physical therapy and the patients they serve,” said David Scala, APTA senior specialist of congressional affairs. “We need to seize the momentum on telehealth and make it clear to lawmakers that maintaining it as an option for Medicare beneficiaries is the right thing to do.”
Get Involved
It’s time to make telehealth a permanent option for PTs and PTAs. APTA makes it easy to add your voice to the effort: PTs, PTAs, students, patients and others can send messages to lawmakers by way of the APTA Patient Action Center. Just follow the instructions for contacting members of Congress.
Joy Bonala
March 18, 2021
When the COVID-19 pandemic reached the small, rural town of Kingstree, South Carolina, Sandra Epps watched her tight-knit community grapple with the devastating disease. Before long, several of her own friends had lost their lives to the virus.
“It was heartbreaking,” Epps said. “It just impacts you in a lot of ways.”
Epps decided to get tested for COVID-19 after realizing she had mild symptoms. She was tested through the Medical University of South Carolina and was contacted immediately about her positive result. Along with the information about her test result, Epps was given the option to be monitored remotely by nurses located at MUSC.
Remote patient monitoring is a virtual care program that allows patients to be monitored through telehealth, while they stay in the comfort of their own home. By logging on to her patient portal, MyChart, Epps could answer questions about her symptoms. Nurses would contact her by phone or email to check in, give advice, and provide reassurance. Epps said the monitoring program made her “feel safe.”
“I was reassured and I wasn’t as frightened,” Epps said.
The novel coronavirus pandemic, which has killed more than 7,800 people in South Carolina, led many healthcare systems to adopt remote patient-monitoring models in an effort to keep hospitals from being overwhelmed.
For patients, remote patient-monitoring allows nurses to monitor symptoms closely and react quickly if needed, according to Dr. Marty Player, Associate Professor of Family Medicine and Co-director of Primary Care, Telemedicine at MUSC.
“We’re keeping contact and accountability with our patients in a much more timely way,” Dr. Player said.
Knowing that a caregiver is accessible has eased patients’ anxiety, he added.
Many of the patients who have been monitored remotely have said the virtual program prevented them from visiting the Emergency Department or an Urgent Care, according to David Wheeler, telehealth patient and provider experience coordinator at the MUSC Center for Telehealth.
“They were able to get through any kind of crisis or spike (in their illness),” Wheeler said. We were able to shepherd them through that.”
After a year of moving IT heaven and earth to enable a huge jump in telehealth services for veterans during the coronavirus pandemic, officials from the Department of Veterans Affairs (VA) said March 23 that one of the biggest remaining obstacles to delivering telehealth is a lack of sufficient and/or affordable broadband service in areas where some veterans live.
VA’s success in ramping up telehealth services during the pandemic has been well documented, with daily service capacity rising ten-fold by mid-2020, to 35,000 appointments per day and the ability to hold 17,000 concurrent sessions. By February of this year, VA was averaging 45,000 telehealth visits per day, up from just 2,500 per day in March 2020.
With firm plans to keep moving forward with telehealth into the post-pandemic era, VA officials said at an event organized by AFCEA Bethesda that a lack of robust broadband infrastructure – along with affordability and service uptake issues among some veterans – represents a big hurdle to further progress.
“One of the biggest telehealth challenges is covering the digital divide in rural areas,” said Jack Galvin, Associate Deputy Assistant Secretary, OI&T Information Technology Operations and Services at VA.
Dr. Kevin Galpin, Executive Director, Telehealth Services, Office of Connected Care, at the Veterans Health Administration (VHA), agreed. “The digital divide is by far the number one issue that we are encountering and dealing with,” he said.
“We have a lot of veterans for whom it’s hard to get affordable internet … or they don’t subscribe” to the service, said Galpin, who cited a 2019 Federal Communications Commission (FCC) finding that 15 percent of veterans don’t have broadband service.
Galpin explained that veterans can be directed to the FCC’s Lifeline program to get subsidized broadband service, or that VA can provide veterans with 4G connected tablet devices in order to receive telehealth services. The agency, he said, has purchased more than 100,000 of the devices to distribute to veterans.
“It’s probably the biggest barrier – just making sure that everyone in this country is connected,” Galpin said. “It’s a crisis … for those that don’t have [broadband service], it’s a real big problem.” He added that VA is excited to work with the government and private sector firms “to get people to the right side of the divide.”
Locking in Pandemic Gains
Elsewhere during the March 23 event, VA officials explained they are looking to make permanent the agency’s pandemic-era gains in telehealth and other veterans services, and then press on with additional IT-driven service improvements going forward.
Galpin said that VA’s various telehealth programs logged 5.6 million “episodes of care” for veterans in 2020, and have “become an integral part of how we deliver services.”
“The vision of our office is to enhance the accessibility of healthcare to patients and caregivers … and bring care closer to the veteran,” he said. During the pandemic, he said, VA showed “how flexible the organization was in the complete pivot of the care delivery model … Everything had to be scaled and pivoted … to see an organization do that in such a nimble fashion needs a spotlight shined on it.”
Galvin said the quick pivot in care models benefited from brushing past “the bureaucratic things that used to hold us back.” The conditions brought on by the pandemic, he said, “really brought to the forefront of what the art of the possible was … and shows what we can do with the right impetus.”
“The new functionality was delivered very rapidly … I think it’s here to stay,” Galvin said.
Dr. Ryan Vega, Chief Officer, Healthcare Innovation and Learning at VHA’s Office of Discovery, Education, and Affiliate Networks, credited the sharp ramp-up in VA telehealth programs during the pandemic as “the only way we were able to reach veterans for chronic care.”
In addition, he pointed to the agency’s work in improving customer-facing websites to deliver healthcare information to veterans. Those efforts, he said, “sometimes are below the surface, but they played out to be incredibly vital” to overall service delivery during the pandemic. “It was all of those pieces that came together,” he said.
Galpin said the quick move to telehealth services was greatly helped by planning that VA started in 2018 with the goal of delivering more care to veterans in their homes by 2021. When the pandemic hit, much of the service pivot “was accelerating what we were doing.”
“It was part scale, and part pivot,” he said, adding, “we had a lot of the platforms in place that we could move from.”
“You can’t wait for an emergency and then think you are going to do it well,” he said.
Shaun Robinson
Boston University Statehouse Program
Published 4:40 a.m. ET Mar. 18, 2021″
BOSTON – Outer Cape Health Services runs three clinics in one of the state’s most rural coastal areas, but for much of the past year, many of their patients have sought care from home. Some are measuring their blood sugar levels on a clinic-provided monitor; others are phoning in for behavioral medicine.
The organization, which has locations in Provincetown, Wellfleet and Harwich Port, took a financial hit and furloughed staff last spring as the number of in-person visits fell, said Pat Nadle, Outer Cape Health Services CEO. Still, Nadle said, remote care is going to stick around as patients come back in. The technology may even help doctors serve them better.
Remote care may help doctors serve patients better
In rural Massachusetts communities from Nantucket to Berkshire County, local health care providers are playing a critical role in the state’s fight against COVID-19. Yet, many of these facilities, which already were operating on thin profit margins and with small staffs, have faced outsized challenges as patients canceled elective procedures and doctors took on additional responsibilities.
Now, as vaccines are rolling out statewide and a new, post-pandemic normal is in sight, advocates say rural health care centers need strong support from local residents and lawmakers. In addition, advocates say, expanding access to telehealth, which lets doctors reach patients safely in underserved areas, is critical.
“They’re not just providing quality health care, but they’re also an economic driver in the community,” Ann Marie Day, executive director of the New England Rural Health Association, said of programs such as Outer Cape Health Services. “They provide a lot of jobs and bring a lot of folks to the community to work, so it’s really important to be able to invest in those rural safety-net providers.”
Statewide, hospital profit margins fell about 4.5% by the end of June 2020, compared with the same time a year earlier, according to the most recent data from the Center for Health Information and Analysis. Less than half of hospitals were in the black, the center found, and the median total margin was -0.7%.
Community hospitals, which serve many of the state’s most vulnerable communities, were among the hardest hit, the data shows. They reported a roughly 7.5% drop in profit margins, and a median total margin of -4.8%. Without government support, the report states, facilities would have gone deeper into the red.
Hospitals in Massachusetts received about $1 billion in federal funding and about $160 million in state funding through the end of last June, according to the report.
President Joe Biden’s approved COVID-19 relief plan includes $8.5 billion of funding for rural hospitals and health care centers to cover expenses and lost revenue as a result of the pandemic. The plan also will provide $500 million for Department of Agriculture grants to rural providers.
“Support from the state and federal government has helped our community hospitals survive this crisis,” Steve Walsh, president and CEO of the Massachusetts Health & Hospital Association, said in a statement. “We remain in close contact with our elected officials to ensure these providers have the resources they need moving forward.”
Providers also have benefited from a state law signed in January requiring insurance companies to provide equal coverage for telehealth and in-person visits, or what is known as coverage parity.
Telehealth lets doctors safely reach patients in underserved areas
Andrew Solomon, senior program manager for Northeast Telehealth Resource Center, said while remote care has helped rural hospitals reach patients for decades, the need for social distancing, as well as legislation like the commonwealth’s parity law, have made the technology more ubiquitous and accessible.
For patients who have a disability or live in areas with limited transportation options, Solomon said, telehealth is a vital tool that enables access to care. Patients who live in small communities may not want to be seen receiving treatment and so prefer the privacy of telehealth, he said, and in some cases, a virtual emergency room visit can provide more timely care than an in-person visit would.
“Providers who hadn’t adopted telehealth before are seeing benefits like reduced no-shows, and those kinds of things are big drivers for providers,” Solomon said. As demand increases and “consumers get more familiar with the potential benefits,” he added, “there will continue to be big drivers there.”
Day, of the New England Rural Health Association, said one challenge for rural telehealth care continues to be limited broadband internet and cellphone connectivity. This is why it’s important that insurance covers telephonic visits, she said, since all that some households may have is a landline.
In 2016, the state identified more than 40 towns in western and north central Massachusetts lacking residential access to broadband. Towns can apply for state grants to build municipally owned networks.
What is telehealth?
“Telehealth is a very broad term,” Solomon said. “There’s a lot of applications and use cases within that, that range from the on-demand live video to remote patient monitoring to provider education opportunities.”
Solomon said telemedicine also allows for joint consultations between primary care providers and specialists, which can help save patients’ time. For instance, he said, a primary care doctor could take a picture on an iPad and send it through a secure platform to a dermatologist; the latter could then decide whether the patient could be treated where they were or whether they required more advanced care.
“Specialists don’t drive out to the Outer Cape much,” said Nadle, of Outer Cape Health Services. “To be able to ‘Zoom’ into a specialist in the treatment room, while you’re in there with your primary care provider, is certainly an option right now to help coordinate care in a much different way.”
Day said rural medical providers also are important vehicles for getting COVID-19 vaccines out to isolated and vulnerable people in their communities. Outer Cape Health Services is distributing about 600 to 800 shots per week across each of its clinics, Nadle said.
In addition to the vaccine rollout, Nadle said, the organization is expanding support for victims of substance abuse who may have been especially struggling with the stressors of the pandemic. Behavioral health care has worked well as a remote service, she said.
At Athol Hospital in northern Worcester County, one takeaway from the pandemic has been the importance of staff collaboration, said Dawn Casavant, vice president of external affairs for the hospital’s parent organization, Heywood Healthcare. Senior leadership and managers have started holding daily meetings to share updates from across the hospital’s departments, she said.
Athol Hospital is a critical-access hospital, a federal designation given to some rural hospitals in remote areas.
“The intersection of all of the primary areas that allow a hospital to function was exaggerated by 1,000% when you’re in a pandemic,” Casavant said. “It’s proven to be really worthy and beneficial for the system to have that opportunity every single morning to start the day on the same page.”
– Amazon has announced the nationwide launch of its telehealth platform, with plans to expand the service from its own employees to other companies.
The Washington-based retail giant announced today that its Amazon Care service, until now limited to employees and their families in its home state, is now available for other Washington companies, and that the platform will be expanded to Amazon employees and other companies throughout the country beginning this summer.
Finally, the company announced that it would offer in-person care to Washington DC, Baltimore and other cities in the near future.
The long-rumored announcement puts Amazon securely in the middle of the retail telehealth sandbox, with a virtual care platform that could appeal to a wide range of businesses. It is expected to compete in a crowded connected health space with vendors like American Well and Teladoc, as well as with payers and health systems offering their own branded programs.
“By supplying Amazon Care as a workplace benefit, employers are investing in the health and well-being of arguably their most important asset: their employees,” the company said in a press release. “Amazon Care enables employers to provide access to high quality medical care within 60 seconds for employees, including options for care around the clock through messaging or video. Amazon Care gives instant access to a range of urgent and primary care services, including COVID-19 and flu testing, vaccinations, treatment of illnesses and injuries, preventive care, sexual health, prescription requests, refills, and delivery, and much more.”
Amazon unveiled the platform roughly 18 months ago, offering virtual care through an mHealth app and on-demand house calls for employees and their families in Washington. In doing so, the company helped to elevate the direct-to-consumer telehealth market, where retail companies like Google, Microsoft and Apple were beginning to compete with Walmart, Walgreens, Rite Aid, CVS and health systems to capture the attention of consumers who didn’t have primary care providers or who were looking for more convenient ways to access on-demand services.
The coronavirus pandemic has only added to the urgency, pushing more services online and away from hospitals, doctors’ offices and other healthcare sites.
“Amazon Care addresses a wide spectrum of patient needs through its primary care and urgent care offerings,” the company said in its press release. “Patients can access preventive care such as annual vaccinations, health screenings, and lifestyle advice. The service also supports patients’ wellness needs, including nutrition, pre-pregnancy planning, sexual health, help to quit smoking, and more. For immediate needs, patients can use Amazon Care to assess and treat illnesses and injuries on demand.”
The announcement could spur a new round of retail healthcare offerings or telehealth partnerships, such as the recently announced merger of Doctor On Demand and Grand Rounds.
“This is a very exciting chess move from Amazon Care,” Taqee Khaled, head of strategy and a healthcare consultant for the consulting firm Nerdery, said in an e-mail to mHealthIntelligence. “A lot of folks will look at this on the outside and not realize how extensively Amazon has been preparing for this moment by obsessively striving to serve their own people exquisitely well. In their iterative process, where fast failure is not just expected but encouraged, they have tried and failed as much – or more – than they’ve succeeded. Along the way, they probably learned a lot and tabled several things for future use toward external competitive advantage.”
“That they’re ready to go national with this is a fearsome prospect for other platforms – and commences what will likely be the digital healthcare equivalent of a Hundred Years War,” he added. “To date, many startups and maturing companies play in this space. … But Amazon perfecting the last mile, pharmaceutical management, virtual care, and – yes, expect it – brick and mortar, may truly mean ‘the end (of traditional health systems) is nigh.”
The Covid-19 pandemic has decimated hospital finances, and as a result, rural providers are forced to make key IT spending decisions with limited dollars. Here is a snapshot of how they will prioritize those dollars this year and the federal support they need to survive the ongoing public health crisis.
As a result, many have decided that their 2021 IT spending must focus on areas that will give them the most bang for their buck. These include equipment upgrades, buying new revenue cycle management technologies, and of course, enhancing telehealth.
This emphasis on telehealth is based on the hope that the regulatory changes related to IT that helped them survive the past year will be made permanent.
A snapshot of the financial landscape for hospitals
Though U.S. providers received federal funding via the Coronavirus Aid, Relief, and Economic Security Act, reports on hospital finances paint a grim picture. Even with federal aid, U.S. hospital operating margins fell 42.4% from last January, according to a February report by Kaufman Hall.
Despite these bleak numbers, many large, urban health systems fared surprisingly well. Several of the most prominent organizations in the country posted billions in revenue last year, like Pittsburgh-based UPMC and Nashville, Tennessee-based HCA Healthcare.
Nearly half (46%) of rural hospitals have a negative operating margin, according to a report by The Chartis Center for Rural Health published last month.
Key IT priorities for rural providers
Against this economic backdrop, rural hospitals have to make IT decisions very strategically, said Brock Slabach, vice president of member services at the National Rural Health Association, in a phone interview.
A major challenge for these providers last year — which is expected to persist this year — is equipment upkeep and the upgrades required to maintain their EHR presence, he said.
“[Rural hospitals] got started with the tremendous subsidies that were afforded to allow them to implement EHRs, and now I’m afraid, many are buckling under the pressure of the investment they made 10 years ago — trying to keep up in terms of hardware and software,” Slabach said.
The subsidies were provided via the Health Information Technology for Economic and Clinical Health Act, passed in 2009. The act created a $27 billion incentive program to urge EHR adoption among hospitals and physician practices. Though the funds helped drive the initial adoption of the technology, now with the requisite upgrades, rural hospitals are on their own.
Though it is difficult to estimate the cost of these upgrades — as it depends on several factors including how much of the hardware has to be replaced or upgraded — Slabach has heard figures ranging from $100,000 to several million dollars.
But, despite this steep cost, a healthy IT infrastructure is key as the move to virtual care speeds up amid the pandemic. So Slabach expects to see continued investment in technology upgrades and updates.
Operational efficiency is also on the top of the list. For Memorial Regional Health in Craig, Colorado, IT investments will be focused on boosting revenue cycle management.
“The faster you process a claim and get it out the door, and the better that technology works, it gets to the payer faster,” said Andy Daniels, CEO of the 25-bed hospital, in a phone interview. “On the backend, once you receive the payment, the faster you are able to post that, your accounts receivable goes down and your cash flow remains stable.”
Steady cash flow is especially necessary for survival in an environment where patient volumes remain uneven.
Memorial Regional Health had outsourced its billing processes prior to the pandemic and had partnered with a bank to assist with collections. Both moves held them in good stead as the public health crisis worsened, Daniels said.
This year, the hospital is considering purchasing payer contract management technology for their commercial clients, he said. This technology will help Memorial Regional Health ensure they are getting reimbursed accurately and in accordance with their contracts.
It’s not just backend hospital operations that are a focus for IT investment. Rural hospitals are hopping on the telehealth train as well — a necessity in the age of Covid-19.
Soon after the pandemic hit, the Centers for Medicare and Medicaid Services implemented several waivers to support telehealth delivery in rural areas.
One of the biggest changes made by CMS is allowing rural health clinics and federally qualified health centers to be reimbursed as “distant sites” when providing telehealth services to Medicare patients during the pandemic.
Previously, these facilities could only be reimbursed as the “originating site” of service for telehealth, meaning they could only get paid for connecting their patients virtually with urban centers for second opinions or consultations with specialists, said the National Rural Health Association’s Slabach.
With the waiver, rural health facilities can also be reimbursed for serving as the distant site of service. This means patients can use telehealth to connect with them from home for care the patient would have usually received in-person.
While this change is positive, rural hospitals had to quickly implement telehealth services to take advantage of the waiver.
“One of the biggest challenges [for rural facilities] was standing up provider-to-patient home telehealth visits after the CMS telehealth waivers were announced,” said Louis Wenzlow, director of health IT and strategic initiatives/CIO of the Rural Wisconsin Health Cooperative, in an email. “Only a subset of rural hospitals had the capacity to engage this, but for those that did, it was a major project.”
At first, hospitals like Memorial Regional Health relied on technologies easily available to them, such as Zoom, Daniels said. But it soon became clear that a formal telehealth strategy was needed, and the hospital decided to add virtual care capabilities via its Epic EHR system.
Memorial Regional will continue to focus on telehealth as a formal strategy in 2021, Daniels said.
“There is no amount of technology to make people come to the doctor,” he added. “They have to feel comfortable to come to the doctor. So, the best thing way [we] can do that is to offer televisits.”
A leader at Clara Barton Hospital, a 23-bed critical access facility in Hoisington, Kansas, echoed this sentiment.
The hospital was not using telehealth at all pre-pandemic, said Michael Thomas, Clara Barton’s IT director, in an email.
“In a rural setting, our patients had never requested a virtual visit because we are literally right down the street from the majority of our patient population base,” he said.
During the pandemic push to digital, the hospital rapidly set up and trained its workforce on a new telehealth solution. Continuing to invest in virtual care solutions for the hospital will be a key even after the pandemic ebbs.
“We quickly realized the technology can be used as a convenience factor for some of our patients, as well as offer a safe environment for our patients to be seen during the pandemic,” Thomas said.
As telehealth deepens its hold on the industry, EHR vendors have recognized that budget constraints may hamper rural facilities’ plans to add this now necessary service.
To help alleviate this burden, Cerner announced last year that it will offer a video visit platform to providers using its CommunityWorks EHR free of charge through the end of 2021. CommunityWorks is a cloud-based EHR tailored to community and critical access hospitals.
“At Cerner, we understand the complexities of health system budgets, especially for critical access hospitals,” said Mitchell Clark, president of CommunityWorks at Cerner, in an email. “Now more than ever hospitals need interoperable technology to help provide seamless care to patients.”
Rural hospitals’ regulatory wish list for IT
Though the end of the Covid-19 pandemic appears within reach, the devastating effects of the once-in-a-century crisis on rural hospitals will likely continue for years to come. Shifts in the regulatory environment will be necessary as these hospitals navigate the new normal.
Rural healthcare stakeholders say that the most beneficial change will be making telehealth waivers permanent.
The government should begin with solidifying telehealth payment parity, said Memorial Regional Health’s Daniels. This would make reimbursement for primary care offered to Medicare and Medicaid patients via telehealth the same as payment for those services in-person.
Though hospital volumes have recovered somewhat, they are unlikely to return to pre-pandemic levels, indicating that telehealth will reign supreme in 2021 and beyond. Telehealth payment parity would help providers recoup the loss from patient volume.
“It’s a volume-driven business for everybody, it just is,” Daniels said. “And [right now] the volume isn’t there.”
In addition, the aforementioned waiver that allows rural health centers to be reimbursed as originating sites of service for telehealth should be formalized, said Slabach of the National Rural Health Association.
And finally, the government needs to ensure that rural areas have adequate broadband access for services like telehealth and remote patient monitoring.
Though the Federal Communications Commission is providing broadband subsidies to eligible providers during the pandemic, this support could be hampered by high demand and limited funding, said Rural Wisconsin Health Cooperative’s Wenzlow. Action needs to be taken to make sure the funding doesn’t run out.
There is no doubt that the Covid-19 pandemic has changed healthcare delivery in this country. But the shift thrusts rural hospitals into an increasingly precarious position. Sound spending decisions, and support where possible, will be necessary to ensure these hospitals not only survive the current crisis but thrive.
Photo: marekuliasz, Getty Images
Media Contact:
Paloma Perez
Congress Tasked the FCC to Create Rules and Procedures for Round 2 of Program to Support Health Care Providers During the Pandemic
—
WASHINGTON, March 17, 2021—Today, Acting Chairwoman Jessica Rosenworcel circulated a Report and Order and Order on Reconsideration that, if adopted, would establish Round 2 of the COVID-19 Telehealth Program, a $249.95 million dollar federal initiative that builds on the $200 million program established as part of the CARES Act. The FCC’s COVID-19 Telehealth Program supports the efforts of health care providers to continue serving their patients by providing telecommunications services, information services, and devices necessary to enable the provision of telehealth services during the COVID-19 pandemic.
“This month marks one year since Americans’ lives were turned upside down as we all began to feel the impact of the COVID-19 pandemic. This crisis has presented extraordinary new challenges and opportunities for patients and providers throughout the country. From patients struggling to remotely connect with a health care professional to manage their chronic conditions, to doctors having to rethink their patient care models, health care providers have had to innovate at a rapid pace. But if the past year has shown us anything, it’s that telehealth technology is here to stay and can be a solution to help address inequities in access to health care services,” said Acting Chairwoman Jessica Rosenworcel. “Late last year, Congress provided an additional $249.95 million to support the FCC’s COVID-19 Telehealth Program. Today I’m proud to advance a proposal to my colleagues to further build on last year’s COVID-19 Telehealth program to support even more doctors and nurses in every corner of our country. Through the COVID-19 Telehealth Program, we can continue to make an impact on the health and well-being of all Americans.”
The Commission fully committed the $200 million appropriated as part of the CARES Act by issuing awards for 539 applications during Round 1 of funding from April 16, 2020 through July 8, 2020. In December 2020, Congress appropriated an additional $249.95 million for the Program as part of the 2021 Consolidated Appropriations Act. In January 2021, the FCC’s Wireline Competition Bureau sought public input on metrics to use when evaluating Round 2 applications, methods to ensure the equitable distribution of these additional funds, and improvements to the application process for Round 2 of the program.
The proposed Round 2 COVID-19 Telehealth Program Report and Order:
- Establishes a system for rating applications, factoring in the hardest hit and lowest- income areas, Tribal communities, health care provider shortage areas, unfunded Round 1 applicants, and more;
- Ensures equitable nationwide distribution of funding so that each state, territory, and the District of Columbia will receive funding since the program’s inception;
- Sets an application deadline to allow for a comprehensive review of all applications in one round, as opposed to the rolling approval system used in Round 1 of the Program;
- Awards funding in two phases in order to satisfy the statutory requirement that applicants be given an opportunity to provide additional information if the application will initially be denied, and to award funding as soon as possible.
To learn more about the FCC’s COVID-19 Telehealth Program, visit https://www.fcc.gov/covid19telehealth.
###
Media Relations: (202) 418-0500 / ASL: (844) 432-2275 / Twitter: @FCC / www.fcc.gov
This is an unofficial announcement of Commission action. Release of the full text of a Commission order constitutes official action. See MCI v. FCC, 515 F.2d 385 (D.C. Cir. 1974).
Click here to view pdf
FILE – This artist rendering provided by Amazon shows the next phase of the company’s headquarters redevelopment to be built in Arlington, Va. The plans released Tuesday, Feb. 2, 2021, features a 350-foot helix-shaped office tower that can be climbed from the outside like a mountain hike. Amazon is making its first foray into providing health care services, announcing Wednesday, March 17, 2021, that it will be offering its Amazon Care telemedicine program to employers nationwide.

